By Drs. Kyle Freese1 and Runa Bakshi2 with Dale Dauten
1Chief Scientific Officer and Epidemiologist, STChealth
2Data Analytics Program Manager, Immunization, Louisiana Department of Health
“What if…?” Putting those two little words together could be the most invigorating sentence-starter in the English language. That’s because those words precede an idea—they represent a new possibility, an experiment, a change. So…
WHAT IF you could test the likely success of your possible vax programs to increase vaccination rates before you ever started them?
WHAT IF you could find out what worked and what didn’t before you ever started implementing in the field? And, importantly, where should you focus your attention to maximize the impact it has on preventing the disease the vaccine is protecting against?
That’s the goal of a new pilot program underway in Louisiana. It began with a determination to take all that happened during the Covid pandemic and find the lessons hidden within, to take the noise and listen for the signals underneath. We are partnering with organizations like Epistemix (a company that specializes in agent-based modeling), and vaccine providers across Louisiana to catalogue successful and unsuccessful vaccine programs and use those findings to build powerful simulations that are both scalable and sustainable.
THE AIMS
Here is what we hope to accomplish…
Specific Aim 1. First, we performed a statewide COVID-19 vaccine coverage assessment by health region (Louisiana has nine of them), focusing on population characteristics, healthcare accessibility, and potential racial/ethnic/ economic disparities.
From here, we determined which regions could serve as a representative sample of the larger state population and compared our findings with the expertise of state stakeholders (more on why that’s important later).
Specific Aim 2. This is where we are now. Over the next two months, through surveys and interviews, we will beengaging key stakeholders to understand the landscape of historical and ongoing interventions and strategies implemented by COVID-19 vaccine providers, including how successful the interventions were in improving vaccination rates. The data collected will be part of the foundation for building our simulation models in Specific Aim 3.
Specific Aim 3. Through our partnership with Epistemix, we will develop agent-based modeling simulations to validate identified, successful approaches and develop recommendations for ongoing outreach efforts. Specifically, these modeling efforts will focus on integrating intervention efficacy information (obtained in Specific Aim 2) with simulations of real communities across Louisiana to anticipate vaccine uptake under different intervention scenarios[AL1] applied to populations with varying community characteristics. And, by extension, the model will help us understand how to minimize disease (i.e. COVID-19) incidence, hospitalization, and death.
THE DREAM
What is the dream here? Picture this:
Once this system is in place, you could sit down with your vaccination program team and
game out different intervention scenarios in a controlled, simulated environment. You’d do this before spending any money, allocating any resources, hiring more people, or disrupting any communities.
Here’s an analogy:
FIGHTER PILOT TRAINING IN A SIMULATOR
Pilots put hundreds of hours in simulator time—much more than the actual mission. Ever stop to think why (other than it sounds like a lot of fun)? It allows them to identify potential weak spots and then practice and perfect their response before getting into a multimillion-dollar machine and going into battle. Not only are those operators better prepared to respond to the practiced scenarios, but they are also better equipped to handle new unknowns. Imagine putting that simulator power at every healthcare and life sciences facility so the decisions they make in their clinics have been simulated over and over—they know how they are likely to play out and how to potentially respond to expected and unexpected hurdles (for example, addressing misinformation or vaccine hesitancy in one way versus another).
THE PLAN
The system we are planning to build will take into account individual characteristics, behaviors, and hundreds of factors about the environment and how the visible (and more importantly, invisible) factors can impact decisions and outcomes. Consider your daily routine: who you live with, the things you do, places you travel, people you interact with, even those you pass on the street. We can simulate that entire environment that operates under well-defined rules. And each of those individuals (we call them agents) has their own set of rules on how they behave when they interact with you. We can modify the environment that those agents live in to simulate any number of scenarios, for instance:
- What would a sudden change in government policy do to impact people’s behaviors for seeking types of health care?
- What if we added a mobile healthcare clinic in Neighborhood X for 3 hours every Saturday by the local high school—would that improve the outcomes we’re interested in, and by how much?
- What if we changed it to 4.5 hours? What about on Sunday instead, and near a church instead of a school?
All of these scenarios are possible, repeatable, and infinitely modifiable.
If you had this information, how would your confidence in decisions improve over time? How much money would you save? How much better could you address health disparities and inequities if only the most effective, efficient, and community sensitive approaches were used? These are the questions we are seeking to answer.
AN IMPORTANT “BUT”
BUT, these models function best when there is community buy-in and participation. This pilot project brings together experts from across the vaccine ecosphere to help guide participant recruitment, data collection, analysis, and dissemination of findings. It follows the model of “patient-centered outcomes research,” which brings stakeholders and patients into the research process from the beginning to identify what outcomes are important to them, how to best engage in communities, and how best to communicate results. But, instead of patients, we are bringing in public health organizations, pharmacies, health plans, schools, traditional healthcare providers, community groups, and many more.
THE CALL TO ACTION: JOIN US!
We would love to include other jurisdictions and organizations in this breakthrough work. So we are creating a Futuring Team that would meet to be informed of progress and to consider ways to adapt and expand the research to eventually help the team members realize their own hopes and dreams. Please let me know if you’d like to consider joining us.

THE TEAM: STChealth visiting with members of the Louisiana Department of Health in New Orleans in November, 2023
STATS OF THE MONTH
Families Getting Immunizations:
Who Has the Time?
By Bill Davenhall, Geomedicine Analyst
Let’s take a look at recent findings from the Pew Research Center on how working moms and dads spend their time.
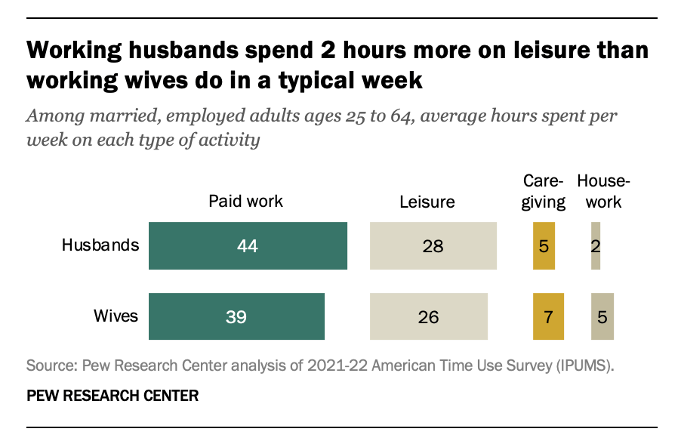
Anyone surprised by these findings?
What then do husbands and dads do with their extra leisure time? According to the researchers, they “relax” and “watch TV” at rates about twice that of their wives. The data originated from The Pew Research Center’s 2012-2022 analysis of the US Bureau of Labor Statistics Time Use Survey. Who knew? (if you’re a husband and father, ask your spouse for confirmation!)
The question now remains, how much time needs to be spent by parents getting and keeping the kids on schedule for all their immunizations? And, more importantly, who will actually make the time to assure that occurs? Leisure and re-charge time is critical in any family raising children, but also critical is making the time to see that the kids are getting and maintaining their immunity.
Making immunizations the least time-consuming preventative health activity that a parent must engage in would, I think, help boost immunization rates across the board. Perhaps more TV and Internet communications directed at today’s busy and time-constrained families would be a place to start—advertising the benefits of immunizations as well as making the act of getting immunizations into children a more equitable activity tradeoff when leisure time is at stake for the three major types of American families raising children. Remember that in 2023 the US Census Bureau reports that there are two other types of “family” households with children under 18: the solo male adult parent household (4.2%) and the solo female parent household (12.3%). Lastly, 51.7% of all family types have no children under 18 present in the household!
Nearly a third of U.S. households (31.7 % or 26.6 million) are married couples with both parents present and children under 18 years of age. Who might have the time to get vaccinations taken care of? The husband-dads own a 2.7-billion hour (that’s right billion) deficit in “caregiving”! That means there is a rather generous potential “gift of time” to see that the kids get all their recommended immunizations on-time!
Two hours a week doesn’t sound like much until you do the math! The table below may help you see what the husband-dad caregiving “time-gift” could be in your favorite state. What a gift that keeps on giving!
As always, I appreciate your 2nd opinions!


0 Comments
Leave A Comment